NEUROSURGERY
Pain Treatment Centers of America is proud to announce we are the first in Arkansas to offer Endoscopic Spine Procedures!
Pain Treatment Centers of America offers a variety of minimally invasive pain treatment procedures that we have perfected to help you achieve pain relief. Our treatments are effective and are at the forefront of pain management. Our goal is to increase a patient's overall function to regain a better quality of life. Below is a list of the surgeries we offer. Please continue reading to learn more about them.
Lumbar Surgeries
Cervical Surgeries
With experts from multiple medical specialties, CLIA-certified labs, cutting-edge surgery centers, and more, Pain Treatment Centers of America has the most combined pain management experience of any practice in the region. Call us at (844) 215-0731 today to learn more about how we can help you find relief from your pain.
Neurosurgeries Offered
Lumbar Surgeries
- Microdiscectomy
- Microforamintomy
- Repeat Microdiscectomy
- Lumbar extra-foraminal microdiscectomy
- Removal of Synovial Cyst
- Sacroiliac Fusion
- Interspinous clamps
- Lumbar or Thoracic Kyphoplasty
- Exploration of previous fusion
- Permanent SCS and trials
- Permanent Pain Pumps and trials
Cervical Surgeries
- Cervical Disc Replacement
- Anterior Cervical Discectomy and Fusion -One Level
- Exploration of Previous Fusion
- Posterior Cervical Foraminotomy and Microdiscectomy
Have Questions?
If your physician believes you may be a candidate for neurosurgery, contact us. We are here to answer your questions, and schedule an appointment when needed.
Meet Our Neurosurgeons
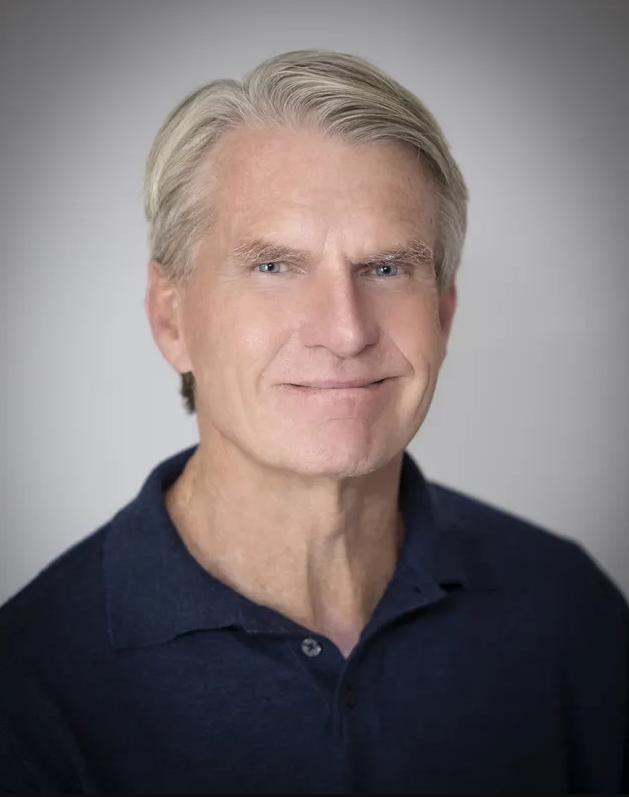
Dr. Mike Calhoun
Dr. Mike Calhoun is an Arkansas native who grew up in Hope and attended the University of Arkansas, Fayetteville. He completed medical school, surgery internship, and neurosurgery residency at the University of Arkansas for Medical Sciences in Little Rock. Dr. Calhoun specializes in spinal cord surgery and peripheral nerves, and his primary practice focuses on the surgical treatment of spinal disorders. The procedures include techniques on the lumbar and cervical spine and lumbar fusion using Minimally Invasive Surgical (MIS) techniques.

Kristen Peek, APRN
Kristen Peek was born and raised in central Arkansas and is a highly experienced healthcare professional with over 25 years in the medical field. Her career has spanned roles from pharmaceutical sales to LPN, RN-BSN, and APRN. She holds a Bachelor of Science in Biology from the University of Central Arkansas, a Bachelor of Science in Nursing from the University of Arkansas in Fayetteville, and a Master of Science in Nursing from Chamberlain School of Nursing.
Referrals for Neurosurgery
Neurosurgery with PTCOA is accepting new patients. Referring physicians will receive regular reports of each patient's progress.
Please feel free to contact us at (844) 215-0731 to setup a referral or fax the Rapid Referral Form to the number below.
Fax a Referral: 888-630-8885







